There is no great genius without a touch of madness? There may be, in fact, a bit of both of them in this attempt to put, in a single text, the (un)definition of madness.
There is no great genius without a touch of madness? There may be, in fact, a bit of both of them in this attempt to put, in a single text, the (un)definition of madness.
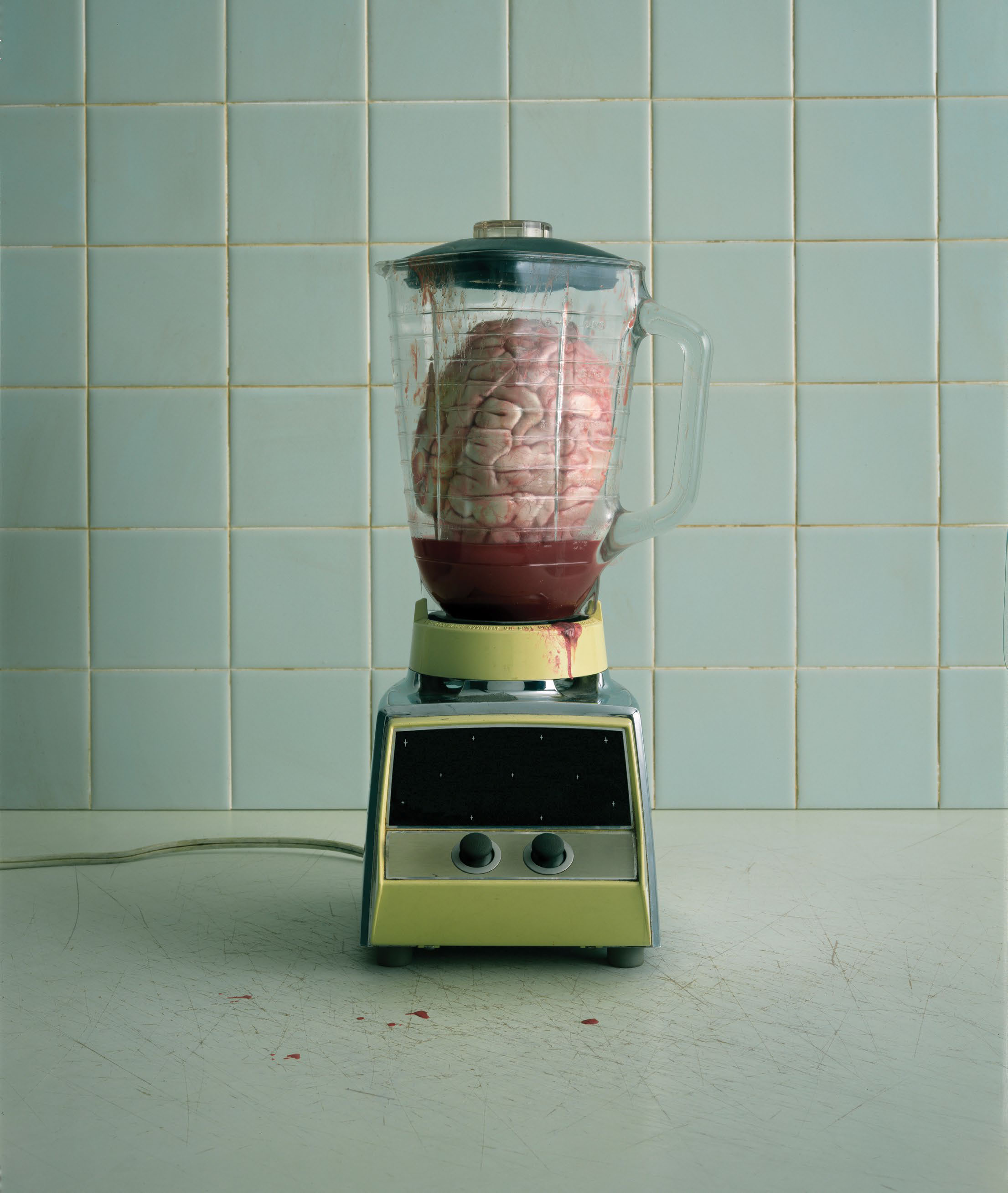
©FOTOGRAFIA: EG PROJECT/GETTY IMAGES
Writing about madness might be, in itself, a bit mad. Because madness implies talking about situations, behaviors and attitudes that go beyond that go beyond what’s considered normal and talking about what’s considered normal is also mad. To talk about madness in the 21st century will certainly have different parameters from talking about madness in any other century, as it will have different perspectives when seen in the light of different social and cultural rules. In other times, it would be insane for a woman to have a right to vote. In other societies, it is still insane for a women to have a driver’s license or certain freedoms reserved only for the opposite gender. For some mentalities and governments, same-sex marriage is (still) madness. For us, for me, for you, none of this should be crazy, its basic human rights, it’s gender equality, it’s something that should be normal and it’s not mad to defend it. What is madness, then? Depends on the perspective? On geography? Social evolution? Is there any consensus in what madness means? Or is it just madness to ask these questions?
Maybe madness isn’t consensual, be it in a social or historical timeline, because madness as a concept is vague. We wear and tear it both in positive and negative references. Wether we’re madly in love or mad for pushing the envelope, metaphorical madness is a matter or intensity, not insanity (though, it may imply a certain level of uncommon or weirdness); in science terms, it’s not even applicable - madness is no clinical term whatsoever, even though many associate it with mental illness, because throughout times, the problems of the mind were seen as a sign of “craziness”. Science came and put each one in its rightful place, substituting the mixed idea for pathologies and diagnosis of disorders linked to the psyche, where the term madness shouldn’t and can’t be used. “In western societies, what is considered madness will be, at least partly, related to the emergency of Cartesian rationality. That is, with the inaugural idea of René Descartes: ‘I think, therefore I am’ (Cogito, ergo sum). This is because Descartes separates madness (illusions and dreams) of the universe from the rational thought: the cogito”, explains Bernardo Coelho, sociologist, researcher and college professor. “More than that, he understands in madness (illusions and dreams) potential ways of deceit of rationality (cogito). And, for Descartes, the cogito (reason) is the great definer of modernity and individuals. Therefore, in western societies, a line is drawn between rationality and irrationality. But, for what’s in question, a line is drawn between reason and madness. That is, a separation between legitimate thought and legitimate thought, between the though we can trust (cogito) and a way of thinking that we should suspect (madness). This border between reason and madness has consequences, maybe the most obvious being exclusion, segregation and stigma related to irrationality - or whatever one finds irrational, unreasonable or mad.” If we were to, then, find here some kind of middle ground, let’s perceive madness, as a society, like a spectrum of group or individual attitudes considered deviant (irrational) from standard behavior, manifesting as violations of social norms and/or that may be dangerous to others or to oneself. But it shouldn't be a definition mistaken with what is scientifically perceived, today, as mental health: “the term madness, as all its synonyms, be it insanity or alienation, are popular terms that come from an age when mental illness was misunderstood, even by the medical community.” Tiago Reis Marques, psychiatrist and Psychiatry professor at King’s College, London, (also won a GQ Men of the Year Award in Science, in 2017), unravels the term from a medical point of view. “Generally, the term madness refers to the lack of an individual’s mental abilities, something that can be secondary to a number of clinical cases and can be present in a temporary or more permanent way, Nowadays, the terms used are more specific and refer to a group of symptoms in which the lack of contact with reality is present. For instance, when feeling delusional or hallucinating. Maybe the medical term ‘psychosis’ is the one that’s closer of what we normally associate and imagine that is madness.” An association that came to us from our ancestors. Madness, to be explored, cannot be dissociated from its perception throughout History.
"But, for what’s in question, a line is drawn between reason and madness. That is, a separation between legitimate thought and legitimate thought, between the though we can trust (cogito) and a way of thinking that we should suspect (madness)." - Bernardo Coelho
In Ancient Greece, madness was considered a kind of voice from the gods, assuming a mythological virtue within the social normalcy. In a time when gods and goddesses were rules over everything, he the were ‘crazy’ established this sort of bridge with the cult, sharing metaphysical informations through abnormal words. It was even believed that the type of madness each one could have would be a decision brought on by the divine. That is, until Hippocrates, considered the ‘father of Medicine’, jumps in. In the fourth century, b.C., give or take, and Hippocrates would ridicule this idea of divine intervention: “If the [patient’s] voice get’s higher, he is compared to a horse and Poseidon is to blame”, he’s point out ironically. “An absurd”, separating for (almost) ever mental illness from the gods and myths and introducing its relationship with the human body, by presenting the four temperament theory, that states that human being’s health condition would be maintained by the balance of four humors, meaning bodily fluids: sanguine (from the heart), phlegmatic (from the respiratory system), the yellow bile (from the liver) and black bile (from the spleen). The unbalance or predominance of one of them would reflect on the temperamental characteristics of each individual. Philosophy also had a role in determining what madness is, with Plato, in the 5th century b.C. making similar assessments to Hippocrates, even before he did, by introducing his theory of soul, consisting of three parts related to the body and mind - reason, emotion and gut feeling -, drawing a similar conclusion to the posterior temperament theory: according to the philosopher, if one of these three was unbalanced, it was mental chaos. The romans came closer to the father of Medicine, accusing the bile of being the vehicle of madness - the yellow one would trigger our manic side; the black our melancholic one. Body and mind, specifically the relationship between them, became the primary duo to comprehend madness and this was the way more or less it arrived our days. Well, except, of course, that chapter in between called the Middle Ages. Anything that was out of the ordinary would be considered a sign of the Devil, because the mind was a philosophical and moral concept and the moral of the time came from God. One feverish episode and the village priest would be called to exorcize - or exile. Depression? Cardinal sin. Sloth? No wonder it’s hellish. The arrival of Renaissance came to change these ideas, particularly with the Age of Enlightenment. At the time, said French philosopher Michel Foucault, the mad were portrayed in art as if they possessed a certain wisdom, like if they knew the limits of the world, and in literature as the revealers of the separation between what men are and what they pretend to be: “It shouldn’t come as a surprise that the surge of institutions specialized in fostering (imprisonment and treatment) of all people considered mad has come only after the emergency of Cartesian thought - it shouldn’t be only because of it, but it will also be because of the emergency of that rationalist point of view of existence and the modern world that one witnesses the birth of these kind of institutions (that first act as a medium of repression imprisonment, punishment; and only later as player of treatment and care)”, frames Bernardo. “It’s important to note that up until the 18th century, European and western societies were used to living with madness - or human behavior deemed as mad - in a relatively inclusive way. I mean, crazy people and the way they expressed themselves, their language and behaviorism weren’t necessarily targets for accusations and stigmatization (let alone reclusion within institutions). Except for violent behavior, which would be repressed.” the approach became, at the time, more rational, though with little advantage for those considered insane, still treated as outsiders: “the opposition between irrationality and rationality debuted by Descartes transforms irrationality and madness in something that’s considered dangerous, a threat, that must be pushed away - like if these people could pollute or contaminate,”, adds the sociologist. “That is why, from Foucault to Gossman, there are references to accusations, stigmatization, and repression of people considered crazy.” Indeed, Foucault admits that “In the serene world of mental illness, modern man no longer communicates with the madman: on one hand, the man of reason delegates the physician to madness, thereby authorizing a relation only through the abstract universality of disease; on the other, the man of madness communicates with society only by the intermediary of an equally abstract reason which is order, physical and moral constraint, the anonymous pressure of the group, the requirements of conformity. As for a common language, there is no such thing; or rather, there is no such thing any longer; the constitution of madness as a mental illness, at the end of the eighteenth century, affords the evidence of a broken dialogue, posits the separation a already affected, and thrusts into oblivion all those stammered, imperfect words without fixed syntax in which the exchange between madness and reason was made.”, he wrote, describing the relationship between reason and madness at the time, in Histoire De La Folie À L'Âge Classique (1961), a publication launched in his first psychology times, born from his own psychological difficulties and experiences from when he worked in an asylum that, at the time, started to cupi the hospitals once destined to the lepers. It was there that, in those days, beggars, madmen, invalids would be put on display, as an example of what would happen to those who would distance themselves from reason. “Madwomen seized with fits of violence are chained like dogs at their cell doors, and separated from keepers and visitors alike by a long corridor protected by an iron grille; through this grille is passed their food and the straw on which they sleep; by means of rakes, part of the filth that surrounds them is cleaned out.”, accused the philosopher. The practice of committing someone in an institution became so common that reporting someone of (not so) erratic behavior was like not taking a bath everyday. Foucault’s narrative, that explores the evolution of the meaning of “madness” in Europe, from the Middle Ages to the 18th century, points out how, at the time, the individual, in his irrationality, would be reduced to an animal condition and the way these institutions would marginalize him for social and political interests, in an attempt to confine “deviant” people and find a “cure” for madness. “In a way, it’s the separation between irrationality/madness and rationality that gives way to social (social construction of madness as a problem) and medical proceedings (emergency and development of psychiatry, etc) that brings defining pathologies for mad or madly behaving people, or outside expected, according to a social and historically pinpointed rationality.”, points out Bernardo Coelho. “In this context of stigmatization of madness, we can almost imagine which current persistence of ways of resisting finding help from mental healthcare professionals or the persistence of social judgement of this who seek them is due to fear of unreason, fear of accusation, fear of being excluded.”, he wonders, arguing a spark for the stigmatization of the matter, still felt nowadays.
Psychiatric revolution arrived more or less at the same time as the French one: in 1793, French doctor Philippe Pinel transformed madness into a medical subject, detaching it from its social genesis, and made it able to being faced as an illness that could be cured, scientifically speaking, and approaching the treatment of psychiatric patients in a more humane and psychological way, through a “moral therapy”. Pinel, responsible for publishing the essay Memoir on Madness (December 11th, 1794) largely contributed for the classification of mental illnesses. In the coming century, Wilhelm Wundt, german doctor and considered one of the founders of experimental psychology, founded the first psychology report in Leipzig, Germany, in 1879, and, in 1899, Sigmund Freud would bring new ground to the area, putting psychoanalysis at the forefront, namely with the publication of “The interpretation of dreams”, an analysis on the personality disorders based on sexuality lived during childhood. Psychiatry, psychology and psychoanalysis took its first steps. The 20th century was prodigal in medical advances on the treatment of mental illnesses, though controversial, specially for contemporary standards: induced comas, lobotomies and electric shock therapy were particularly popular on the thirties, when it was discovered that convulsions were able to ease some of the psychiatric symptoms. But its application was flexible and rudimental: primitive gadgets and intuitive treatments with no prescription of time or intensity, often used as punishment and not treatment, with no anesthesia. Electroconvulsive therapy wasn't in vain, though, it evolved through time and with the help of sedatives for sessions that were more thought of and more human. The era of psychopharmacology begins, which allowed pharmaceuticals to substitute surgical interventions like lobotomies. The arrival of antidepressants, anxiolytics and other kinds of medicines transformed psychiatry as well as the pharmaceutical industry, for the better and for the worse, being some times criticized for relying too much and solely on medication. But the learning didn’t stop. The 21st century, still with lots to learn, brought important researches, namely in what concerns the study of genome and mapping of the brain’s circuits, which has revealed which are the areas involved in disorders like the obsessive-compulsive kind, depression and extreme anxiety, even if the cure is something from the future. It also helped, a lot, to separate the term madness from the medical area. “In clinical terms, nowadays, nobody uses the term madness. Science always felt the need to separate, group and classify the natural world.”, Tiago Reis Marques explains. “That is around since Aristotle, probably the first philosopher/scientist to try and do it. However, the first classifications of the natural world came up only during the Age of Enlightenment with Linnaeus, the father of taxonomy, which is the science of naming and classifying animal and plant species”, the psychiatrist refers. “Psychopathology is the equivalent to taxonomy, but for the world of psychiatric illnesses. Psychopathology allows us to identify the different psychological phenomena (symptoms) that emerge from mental illnesses. By knowing the different psychic symptoms, we can then identify, afterwards, the mental illness, in the same way as, by identifying physical symptoms, we are able to tell the organic diseases that each individual suffers from. There are apsçp studies that identify genes that can cause the malfunction of the neural circuits, though relating genes and disorders is far from being simple. “The brain is the most complex organ of our organism and is, therefore, the hardest one to study.” points out Reis Marques. “This means that all brain illnesses are inherently hard to understand. On the other hand, most mental illness leave no brain ‘bruises’, there is no cerebral alteration that is relevant or specific of the illness. That distinguishes them from other brain illnesses such as Alzheimer, where there’s a deposition of amyloid plaques, or epilepsy, where there’s a change in the electric activity of the brain easily observed in an electroencephalogram. The changes that, today we know to exist in mental illnesses are much more subtle, diffuse and, thus, hard to study. Also, there are multiple causes for mental illnesses, and it hasn’t been possible, yet, to find a common denominator, a unique mechanism that explains these illnesses. We are still trying to understand the causes, the mechanisms and the neurobiology of mental illnesses. Only like this we’ll be able to continue adding pieces to this puzzle and better understand these diseases.” Even with a long way to go, evolution, discovery wise, has been extraordinary - as well as fighting the stigma - even if still very much around and far from being healed. And it all starts with the idea that madness cannot be confused with mental illness: “the term madness Is totally non-specific and gives us no info whatsoever about what’s going on with a certain patient. It is, therefore, and incorrect term and, unfortunately, has a negative connotation”, specifies Reis Marques. Which doesn’t mean that what we perceive as madness cannot be triggered by some sort of disturbance of the mind, assuming madness is the manifest of a dissociation from social norms.: “In clinical terms, we can identify a group of symptoms and behaviors in which there’s a breach of contact with reality. There are several mental illnesses in which that can occur, like for example in bipolar disorder with psychotic symptoms, in severe depression or in schizophrenia. Each of these clinical cases has a specific presentation and a different level of severity. It’s ok to say that the so-called madness might be cause by a diverse set of mental illnesses, each one with a different level of seriousness.” But how to tell if we’re facing a mind disorder if we’re simply in a more, metaphorically speaking, mad phase? How can it be diagnosed? “Mental illnesses diagnose is still made completely through clinical query, which allows us to identify the different mental symptoms (the aforementioned psychopathological phenomena), and fit them in specific clinical context cases”, Tiago explains. “Obviously, advances in Science will allow, sooner or later, resorting to auxiliar methods of diagnosis to identify and characterized in a more detailed manner mental illnesses. This is already done in several cerebral pathologies. (…) The brain is complex in such a way that we haven’t yet the tools to diagnose brain diseases appropriately. All diagnoses is still done entirely from clinical observation. We hope this changes in a near future.”
“The term madness, as all its synonyms, be it insanity or alienation, are popular terms that come from an age when mental illness was misunderstood, even by the medical community.” - Tiago Reis Marques
The prospect of new discoveries and advances in this area is, more than ever, a priority. Stress, life in the fast lane, anxiety of “everything is possible” and disappointment over “everything is actually not possible” have made the 21st century an era ruled by the damages of the psyche and nervous system. Mental illnesses are already the tragedy of our times, confirms Reis Marques: “Five mental illnesses are on the top 20 of illnesses that are more limiting. In terms of years lost due to inability, mental illness is neck and neck with cardiovascular disease, for instance. Overall, it’s estimated that one in four people will suffer from a mental illness throughout her life span. several factors are associated with life in the 21st century, like city life, social pressure, excessive stress, sleep deprivations, bad eating habits, lack of physical exercise, too much time spent in social media and the absence of family and social ties are all significant risk factors for mental illnesses. It’s important that there is work towards identifying and reducing these risk factors. Within all mental illnesses, depression and anxiety pathologies are the ones that prevail the most. Nevertheless, sleep pathologies, eating disorders and addictions are rising ones. It is fundamental, so as to prevent an epidemic of mental illnesses in a near future, betting on prevention and learning how to take care of this wonderful organ that is the brain!”, warns the doctor. A mission with many challenges, because “understanding the organization and way of working of an organ with 86 billion neurons and approximately 100 trillions synapses is a huge challenge that, though, little by little, has been conquered, it’s still far from being accomplished.” And adds: “without understand the workings of the normal brain and what’s going on in a brain with a mental pathology, it becomes a huge challenge to try and develop new therapeutical solutions. That is the reason why many new drugs have failed in clinical tests. There are, however, reasons for remaining optimistic, as the last years have been characterized by an impressive investment and emergency of new very promising molecules. In the case of depression, we see the arrival in the market of ketamine and an effective therapy for depressions that resist treatment. Some psychedelic substances, like psilocybin, also seem pretty promising. In the case of schizophrenia, a group of molecules are now in the final stages of clinical tests. I would say the next years will be punctuated by the emergency of several pharmaceuticals that will substantially increase the existing therapeutical arsenal. Nevertheless, we will have to invest heavily in neurosciences to better understand the brain so that more and better treatment alternatives can be unveiled.”
And we really need for it to happen, and we all have a bit of madness within ourselves - be it because of external factores, be it for genetics’ reasons. Yes, it is possible to “inherit” some “madness” or have a “madness gene”: “I’d say there are many madness genes, not only one!” replies the psychiatrist. “All mental illnesses are polygenic, which means there are multiple genes as risk factors for these mental illnesses, there is no mental illness there is simply attributed to one single gene. In the case of schizophrenia, the disease most commonly associated with madness, there have been identified already more than 100 genes that are risk factors for it. The evolution of genetic has allowed us to identify each of these genes and understand in which way they can enhance the risk of having the illness. By understand the role of each one of those genes, we’re able to pinpoint in which way the product of these may explain the disease. That’s how we identified that in schizophrenia, many of the genes involved in the immune response bring simultaneously an added risk of the illness. that was a basis for one of the the most recent theories about the neurobiology of schizophrenia, which is the inflammatory theory, which, on the other hand, brought us to attempting to use potent anti-inflammatory medicine in the treatment of this illness. It’s a perfect example of how genetic studies can contribute to the comprehension of the disease and development of new treatments”, adding that “most mental illnesses have a significant genetic component, be it bipolar disorder, schizophrenia, depression or Alzheimer. It is, however, important to clarify that the fact that there is a genetic component doesn’t mean it will manifest itself. We have to think of the genetic component as a risk factor and that its presence will increase the likelihood that a certain illness will manifest itself. Let’s look at depression as an example. The risk of having a depression, if there are no relatives affected by it, is about 10%. But if you already have a relative with depression, like a father or brother, the risk rises to 20 to 30%. meaning the genetic component will increase the risk in more or less two to three times mor likely to have it. Obviously, inheritance varies from illness to illness and also according to the genetic proximity to the relative. (…) So, what contributes to the risk of mental illnesses besides the genetic component? The other variable is environment, that is, everything that the individual is exposed to throughout his life, like stress, traumas or access to drugs. Even though there’s nothing we can do regarding our genetics, we can control the way we expose ourselves to environmental risk factors, and thus protecting our brain, avoiding mental illnesses from manifesting themselves.”, advises Reis Marques. In fact, wrote Foucault, referring to the alliance between deviating from normalcy and the loss of reason, and quoting “Matthey, a Geneva physician very close to Rousseau's influence, formulates the prospect for all men of reason: 'Do not glory in your state, if you are wise and civilized men; an instant suffices to disturb and annihilate that supposed wisdom of which you are so proud; an unexpected event, a sharp and sudden emotion of the soul will abruptly change the most reasonable and intelligent man into a raving idiot.’” And that event or emotion can happen to any of us. “These external factors are important risk factors for mental illnesses”, adds the psychiatrist. “We now know that many can trigger these diseases. In some cases, the association is very direct and immediate, like in the case of drugs, for example. Cocaine increases the release of dopamine, and the excess of dopamine can provoke a psychotic surge. Same thing happens in the case of acts stress, that can trigger a panic attack. In other situations, these external factors provoke subtle changes that only afterwards can cause mental illness. In children, bullying or verbal violence can provoke changes in the neurodevelopment which, in turn, may lead to a higher risk of mental illness in adulthood, like depression or schizophrenia. In this case, the external risk factors precede in several years the manifestation of the disease.” That is why it is so important to identify factors to identify treatment.
And speaking of treatment, it is also imperative to talk about the way mental illnesses are perceived, socially speaking. The stigma surrounding mental health isn’t smoothing form ages ago and, even though we know “mad” is not at all what meant in other eras, we are still far from understanding that mental disorders are real, stigmatizing them by downplaying them - not realizing the full extent of its seriousness - or by misunderstanding them, marginalizing them because they result in uncommon behavior. “The stigma surrounding mental illnesses is still very much present and prevailing. There’s the external stigma, visible in the discrimination of mental patients by society, and self-stigmatization, in which one forms negative ideas about oneself just because one suffers from mental illness. (…) Similarly to any other stigma, this one comes from the ignorante and misconceptions that have been created throughout the years. Traditionally, what is unknown causes fear and that is particularly visible in mental illness. One is afraid of the mentally ill and that lead to the patient being discriminated against, misunderstood and shun from society. This stigma comes from, above all, misunderstanding the symptoms and causes of mental illnesses, something that is fortunately changing, Little by little, we see more an more people owning that they suffer or have suffered from metal illness, normalizing it. We need to talk about mental illness, explain the ways of the brain, support awareness campaigns, a common effort as important as fighting any gender, color or sexual discrimination. It’s unacceptable that someone is still discriminated against for having mental health problems”, says Tiago Reis Marques. What can help? “Change needs to come from not just public and health education, but also legal reforms and awareness campaigns. It’s a long process, but fundamental. It’s the responsibility of each and every one of us to fight any kind of discrimination, let alone one that affects a population as vulnerable as the one that suffers from mental illness.”
"Still today, in contemporary societies, where experimenting is a central aspect of people’s lives, it’s still funny that we refer to some of the stuff we do as madness, simply because they break up with reasonable logic and rational morality." - Bernardo Coelho
Then, what is madness, after all? “We cannot dissociate the evaluation of what is madness or mad behavior from a logic of body control, of expression, and life experimentation”, defends Bernardo Coelho. “that is, in the definition of what is madness or what is mad behavior can also be a moral evaluation of what we do, can and cannot do. Basically, the border between madness and rationality, or between madness and sanity, also touches our ability of self-control and permanent vigilance over the appropriateness of what we do. Still today, in contemporary societies, where experimenting is a central aspect of people’s lives, it’s still funny that we refer to some of the stuff we do as madness, simply because they break up with reasonable logic and rational morality. For instance, many activities to escape the daily rut are considered small crazy gestures. Another examples: in daily speeches, we say that many things we do or certain behaviors we have are mad, which are frequently linked to the feeling of strong emotions, of breaking out of the comfort zone, of pleasure, etc. Meaning, what we say is crazy in our lives are breaches in rationality that rules most of our time.” The spectrum of references is so wide that it’s also mad to think that madness can be defined in just one way. For example, “love is also frequently associated with irrationality and even madness. Until late 19th century (even beginning of the 20th century), it wasn’t uncommon the frequent committing of women in asylum, mental institutions or convents, simply because they manifested their lust. That is, when women’s sexual desire contradicted the rational wants of the family regarding the future of their daughters they faced accusations of madness and eventually being committed in an institution. About this, it’s important to underline the significance of thought and feminist movements - first of all, the suffragist - that came to shine a light on love and loving feeling as a central aspect for women’s lives.
Maybe what is consensual is that it is crazy to keep belittling signs of mental disorders and illnesses, being mild or severe. Like reducing depression to being sad, anxiety to being nervous, having phobias to being afraid. Like treating madness as just a word and use it lightly. Of course we can still use it: it would be mad to use censorship to heal insanity. But it’s in the understanding of its differences that we can define it. And knowing that there’s always, as the term “madness and not as a psychosis, some level of undefinable to it. After all, “the marvelous logic of the mad which seems to mock that of the logicians because it resembles it so exactly, or rather because it is exactly the same, and because at the secret heart of madness, at the core of so many errors, so many absurdities, so many words and gestures without consequence, we discover, finally, the hidden perfection of a language.”, quoting Michel Foucault. There is no great genius without a touch of madness? It would appear so. And even if that dose of madness goes into overdrive, science has made the effort to understand it and ease it. As a society, all we have left to do is embrace it and not stigmatize it. It’s accepting it as human. Accepting it as relative, philosophically peaking, and always conditioned by social normalcy: “Madness is something rare in individuals — but in groups, parties, peoples, and ages, it is the rule.” said Friedrich Nietzsche. And the rule, now, today, should already be, in between you and me and all of us, not to mistakenly see madness and mental illness as the same thing.
*Originally published in Vogue Portugal's "The Madness Issue", from July/August 2020.A versão portuguesa está na edição impressa, aqui.
Most popular
.jpg)


Relacionados
.jpg)
Anna Wintour e o presidente da câmara de Milão, Giuseppe Sala, revelam a localização do Vogue World 2026
24 Feb 2026



O que lhe reservam os astros para a semana de 24 de fevereiro a 2 de março
24 Feb 2026

